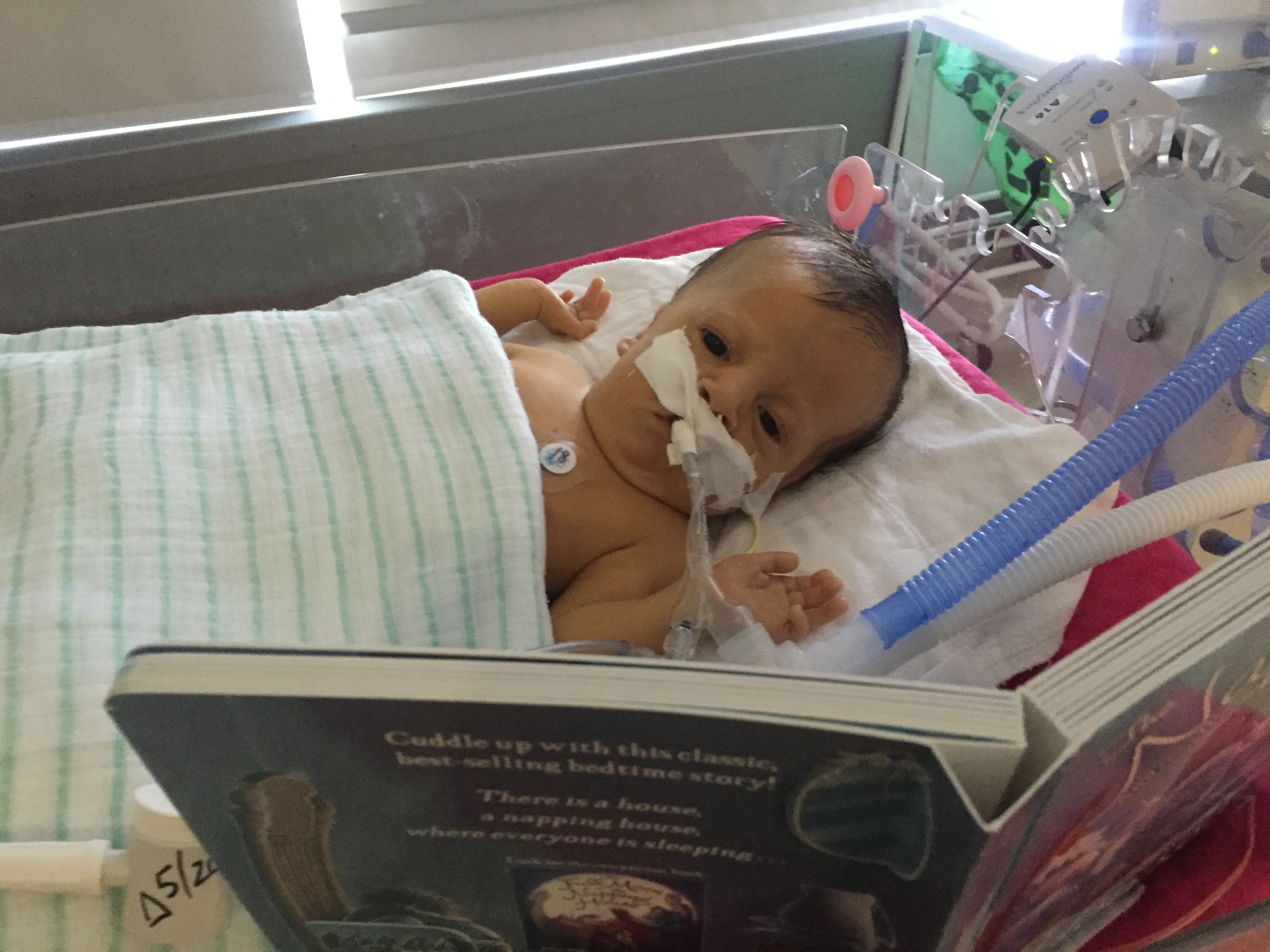
My sweet, sweet, daughter, Olivia. I love her so much.
Every time she opens those big, innocent (and blue!) eyes, I fall in love all over again. I dream of all things I want her to experience, and I think of how far she has come since those early hours on April 24th.
An hour after birth, following continuous “bagging” and eventual intubation to keep her frail body breathing, a medical transport team whisked her from Highland Hospital to the Strong NICU. Before leaving, they rolled her isolette into the delivery room, where Mom & I sat still in shock, to let us say hello for the first time, and goodbye. Sadly that was not the first time we thought we might lose her, but given her birth, her state, and all physical objects surrounding her, this time it felt more real.
It was the first time Whitney has ever seen me cry.
We arrived in the NICU a few hours later, and saw her again from outside her room. She had made it. Her bedside was surrounded by a team of doctors and nurses. The attending doctor stepped out to give us an update, noting that “based on her observable condition, she may only have a few hours or days”.
She’s come so far since those early hours.
However after three weeks, I feel it is important to zoom out for a minute.
Although we cheer every poop, minor change in ventilator setting, and decimal size reduction in bilirubin, we feel it important to admit that no matter how strong she is, Olivia may not be able to overcome this battle. This is not new, nor is it something Mom and I feel is taboo to talk about. We’ve even shared this (in one way or another) with most of you during your previous visits.
So, what do we know?
We know Olivia suffered serious injuries during delivery, but feel relatively confident that these issues are behind her.
The larger, more complex truth is likely an underlying genetic disorder.
This was one of the hardest things for me to accept. During Whitney’s first trimester screening at 12 weeks pregnant, an abnormal NT scan revealed a cystic hygroma on the back of Olivia’s neck. We consulted with a doctor, met with a genetics counselor, and decided to immediately pursue further testing. Mom underwent a chorionic villus sampling (CVS) procedure which removes cells from the placenta to be tested for chromosome abnormalities and other inherited disorders. We waited 5 hard weeks for those results, during which Mom and I contemplated a lot of serious outcomes. This was the first time we thought we might lose her. Even after receiving “normal” results from the CVS, DNA microarray test, anatomy scan, and fetal echocardiography, it took us a while to believe that we were still having our baby. It was an incredibly difficult time.
So, when the doctor’s immediate conclusions at birth suggested possible genetic issues, I was reticent to believe it. After all, the vacuum assisted birth caused significant bleeding in and around her skull, mustn’t that be the cause? But, we now know this is not the case, and in hindsight there were a few indications of this truth, starting with the abnormal NT scan.
While not a clear picture yet, Olivia has presented a number of clues which are helping the genetics and neuromuscular team work towards a diagnosis:
- Her breathing is weak and she can’t breathe on her own.
- Her skeletal muscles are weakened or non-existent. And while not paralyzed in the traditional sense, she can’t actively move much beyond her fingers and her toes.
- Her liver isn’t working correctly (as first indicated by high direct/conjugated bilirubin levels), which could ultimately lead to failure.
- Her digestive track isn’t working correctly. She’s not actively processing feeding and relies on TPN intravenously for nutrition.
- She had temporary kidney issues (SIADH), but at least those resolved.
- She has a moderate ventricular septal defect (VSD) or a small hole in her little heart.
What does this mean?
In medical terms, we do not yet know if we’ll get differential diagnoses (multiple, unrelated issues) or a unifying diagnosis (a single, diagnosable disorder that makes sense of her multiple symptoms). Said differently – everything described above could be related or they could be independent. Understanding the diagnoses (unifying or differential) is important in determining which of symptoms to focus on, which will get worse, and which we have a chance of treating.
To figure that out, in addition to the neonatologists at the NICU, we have specialists from the genetics, neurology, GI, renal, and pulmonary teams consulting on Olivia’s case. There seem to be more every day. These teams continue to visit and asses Olivia, and each have ordered a number of tests which allow us to rule out (or confirm) possible causes. Currently, the leading area for a possible diagnosis is from the neuromuscular team. We are working with an internationally acclaimed pediatric neuromuscular specialist (referred to as Dr. C in our updates).
Dr. C suspects (via clinical observation) Olivia has a syndrome of the peripheral nervous system (PNS). This means that her brain and spine (CNS) are producing and sending the right signals to control her body. But, somewhere in the nerves or the muscles, those signals are not getting to their final destination. [Edited to note: Olivia’s muscle biopsy later revealed this long held assumption to be incorrect. You can read more about her final diagnosis of Spinal Muscular Atrophy.]
The range of possible conditions in this area is vast and not easily diagnosable. Some are rare – having only 60ish confirmed cases in the world – while others are commonly known. She’s not an obvious shoe-in for any.
Dr. C is working closely with Dr. F (genetics) to piece together the symptoms and clues Olivia has so far presented in order to narrow in the search for potential causes. They have ordered a next-generation sequencing of her genome to look at the 127 genes known to express PNS related conditions. There is a real possibility, however, that even with all the progress of modern technology, DNA testing at this level is still a few years away from being able to isolate her condition. Dad, the ever wanna-be futurist, knows this all too well.
The other reality is that the outcomes for plausible PNS conditions vary wildly. Just like our first NICU attending told us in the hours after her birth: there are some real chances that Olivia won’t make it. In fact, every time we’ve seen a new doctor here, they take a moment to make sure that Mom and I understand that. We appreciate their frankness.
Of course, there are also survivable and more favorable outcomes. Technology – a la permanent ventilation (or tracheal tube), feeding tubes, and other in-home care options – may provide an enjoyable quality of life with some these. She could also recover from all this one day (OK, that may be Dad just wishing). And who knows: gene therapy, stem cell regeneration, and other advanced technologies could present possible “cures” in the future.
As of now, we can’t draw any conclusions. And we won’t. Mom and I continue to provide daily updates, where we choose to celebrate every poop, every yawn, and every day with Olivia. But we are informed of our possible realities, and we want you to be too.